- Prediabetes Mastermind
- Posts
- Stop managing prediabetes. Start reversing it. Here's why.
Stop managing prediabetes. Start reversing it. Here's why.
New research: blood sugar beats just 'managing' it.
Welcome back, health champions!👋
If you've been diagnosed with prediabetes, what should be your goal—prevent its progression to diabetes, manage symptoms, or reverse prediabetes (what scientists call remission)?
A paper published in a top-tier journal just weeks ago in 2026 analyzed 50 years of combined data across different cultures and continents to provide insights.
In today's Health Guide, we're breaking down:
Better glucose control vs weight loss—who wins?
What "remission" actually means (and the simplified version)
What you should do differently starting today
Can we get your input?
Over the past year, this newsletter has focused on sharing clear, science-based guidance for prediabetes.
Your perspective helps ensure it continues to focus on what actually matters.
We’ve put together a brief 2–3 minute survey.
As a thank-you, one participant will be randomly selected to receive a $50 Amazon gift card.
BEST FINDS
Winter Comfort, Steady Glucose 🍲 Cold weather naturally pulls us toward cozy, hearty meals. Creamy White Bean Soup with Kale, Rosemary & Lemon: Creamy without dairy, rich in fiber, and brightened with lemon for a comforting but light winter soup. Italian Chicken, Mushroom and Barley Soup: A hearty classic with lean protein and barley—a slow-digesting grain that keeps you full longer. Roasted Sweet Potato and Chickpea Bowl: Roasted, spiced, and satisfying—this bowl balances natural sweetness with fiber and protein. Cabbage, White Beans and Spicy Sausage One-Pan Dinner: One-pan comfort with lots of volume, fiber, and just enough spice to feel indulgent. Skillet Lemon Rosemary Chicken and Farro: Bright, savory flavors with chewy farro for steady energy and great texture. Garlic Mashed Cauliflower Potatoes: A lighter twist on mashed potatoes that still delivers on comfort and flavor.
How Reversing Prediabetes Protects Your Health for Decades
If your doctor told you that you have prediabetes, you probably left the office with advice like "watch your diet" and "exercise more." That's not wrong—it's just incomplete.
New research is changing how we should think about prediabetes goals. Instead of just trying to keep it from getting worse, we should be aiming to get blood sugar back to normal levels. And the data shows this isn't just feel-good advice—it's backed by decades of evidence showing dramatically reduced heart risk.
We're talking about research that followed nearly 3,000 people with prediabetes for 20 to 30 years.
The Two Studies That Tracked Prediabetes for Decades
Two major research trials tracked what happened to people with prediabetes over an incredibly long time:
Study 1 (USA): 2,402 Americans followed for over 20 years
Study 2 (China): 540 Chinese participants followed for over 30 years
Why does it matter that these studies included different populations? Because it means the findings aren't just relevant to one group of people—they worked across cultures, continents, and time periods.
The bottom line: 2026 article shows that people who achieved remission (got their blood sugar back to normal) had roughly half the risk of cardiovascular death or hospitalization for heart failure compared to those who didn't achieve remission.
And here's the remarkable part—this protection lasted for decades, even after the intensive intervention period ended. Scientists call this a "legacy effect." You put in focused effort for 1-6 years, and your heart stays protected for 20-30 years.

Understanding Prediabetes Remission—What It Really Means
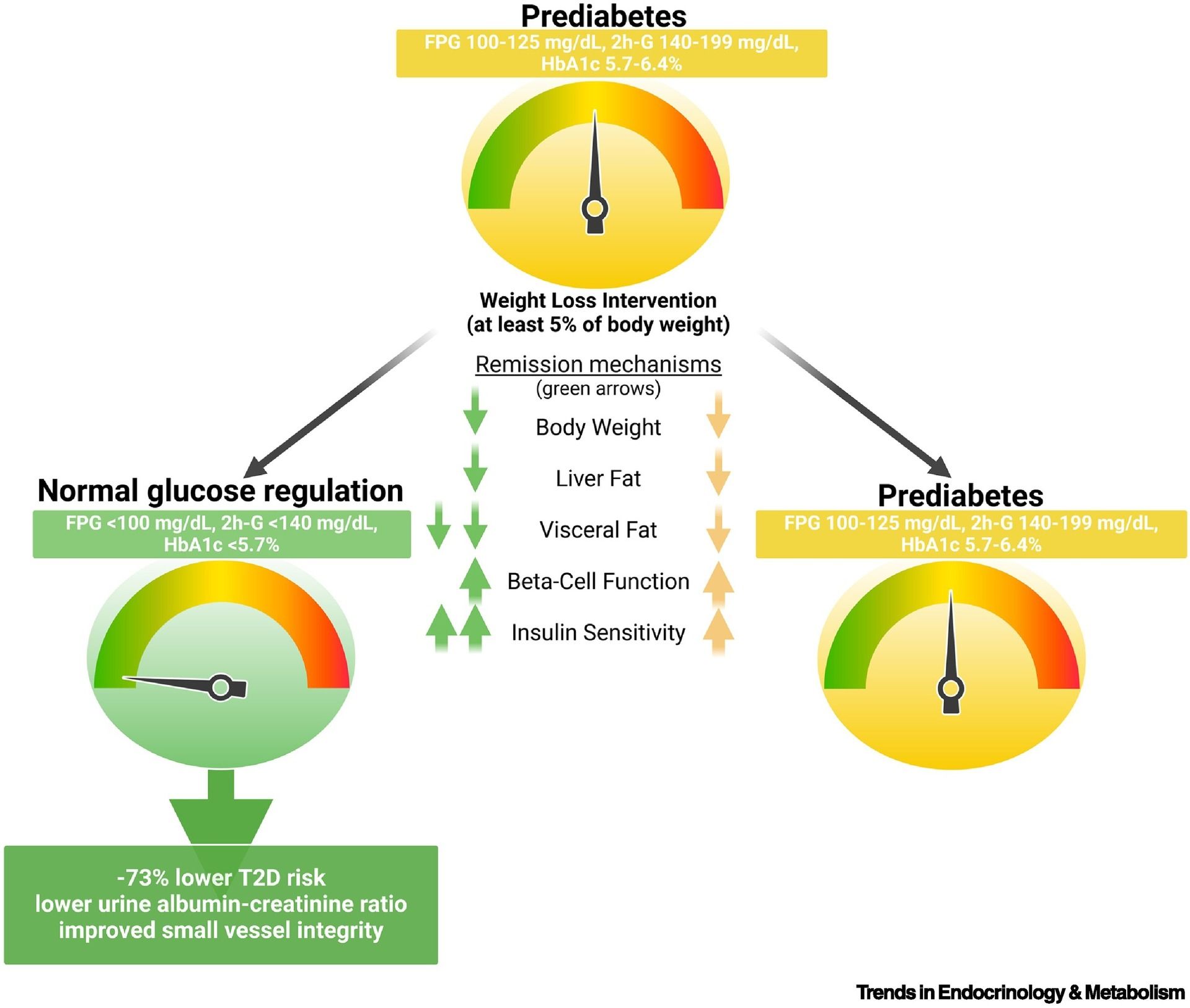
Let's get specific. Remission means hitting all three of these blood sugar targets:
Fasting blood sugar: Below 100 mg/dL
2-hour glucose test: Below 140 mg/dL (after drinking a sugar solution)
HbA1c: Below 5.7%
The simplified version: A fasting blood sugar of 97 mg/dL or lower captured most of the heart-protective benefit.
That's one blood test your doctor can order at your next visit. Easy to measure, easy to track.
Blood Sugar Control vs. Weight Loss—The Surprising Winner
Here's where things get interesting.
The people in these studies focused on weight loss (aiming for 7% of body weight) and exercise (150 minutes per week).
Research shows that weight loss alone doesn't guarantee remission. In one study, people who lost similar amounts of weight had very different outcomes: those who achieved remission showed greater visceral fat loss, better insulin function, and lower inflammation than those whose blood sugar remained elevated despite weightloss.
The people who achieved remission got bonus benefits:
Better insulin sensitivity (their bodies used insulin more effectively)
Improved pancreatic function (their beta cells, which make insulin, worked better)
More visceral fat loss (that's the dangerous fat around your organs)
Better fat redistribution (fat moved from dangerous visceral areas to safer subcutaneous storage)
Lower inflammation throughout the body
Here's the really interesting part: some people achieved remission without losing much weight at all. Weightloss is important, but it's not the only thing that matters. Getting blood sugar back to normal captures metabolic changes that weight loss alone doesn't always deliver.
What’s your biggest challenge with prediabetes right now? |
Why Current Guidelines Fall Short
For years, prediabetes advice has been defensive: just try not to let it get worse.
Current guidelines focus on weight loss and physical activity, but they don't recommend specific blood sugar targets as prevention goals. This research flips the script. The data consistently shows that getting blood sugar back to normal levels (not just improving it slightly) comes with massive, long-lasting benefits that persist for decades.
The Reality Check: Success Rates and What They Mean
Time for a reality check.
In these studies, only 11-13% of participants achieved remission. That's pretty low, which tells us this isn't simple or automatic.
But here's the thing—those who did achieve it saw such dramatic benefits that it's absolutely worth pursuing. We just need better tools, more support, and smarter strategies to help more people get there.
What the low success rate tells us:
You probably need more than a handout with diet tips
Sustained support matters—think structured programs, registered dietitians, or accountability groups
This is a marathon, not a sprint - achieving remission took 1-6 years of focused effort in these studies
Don't get discouraged by the difficulty—get strategic about your approach
Your Action Plan: What to Do Starting Today
1. Talk to Your Doctor About Remission as Your Goal
Don't settle for "try to manage your prediabetes." Set remission (normalizing your blood sugar) as your explicit target. Your goal should be clear: fasting blood sugar at or below 97 mg/dL.
2. Track What Actually Matters
Yes, monitor your weight. But also:
Get regular fasting blood sugar tests (not just at annual checkups)
Ask your doctor about HbA1c testing
Consider a continuous glucose monitor if it's accessible to you
Pay attention to how different foods affect your energy and blood sugar
3. Focus on Metabolic Health, Not Just Weight
Your action plan should target the deeper changes:
Eat for insulin sensitivity:
Focus on foods that don't spike blood sugar
Prioritize protein, fiber, and healthy fats
Limit refined carbs and added sugars
Move to reduce visceral fat:
Mix resistance training (builds muscle, improves insulin sensitivity) with cardio
Aim for that 150 minutes per week target
Daily movement matters as much as formal exercise
Manage the invisible factors:
Sleep: Poor sleep wrecks blood sugar control
Stress: Chronic stress raises cortisol, which raises blood sugar
Consistency: Sporadic efforts don't create lasting metabolic change
4. Be Patient but Persistent
The people in these studies worked hard during active intervention for 1-6 years. That's significant time and effort.
But they got decades of heart protection in return. That's an incredible trade-off—short-term focused effort for long-term health security.
The Big Picture: Why This Matters for Your Future
Here's what makes these findings game-changing: they show prediabetes isn't a permanent diagnosis you just "manage." It's a condition you can reverse, with clear targets and serious rewards.
For decades, prediabetes felt like a waiting room for diabetes. Talk to your doctor. Set remission as your target—fasting blood sugar at or below 97 mg/dL. Track your progress. Focus on metabolic health, not just the scale.
The questions you're probably asking:
"Is it worth the effort?"
Yes. Cutting your risk of cardiovascular death or hospitalization for heart failure roughly in half for 20-30 years is significant.
"Will it work for everyone?"
The data shows it's possible across diverse populations—different ages, ethnicities, and starting points. Not everyone will achieve it with current approaches, but it's absolutely achievable.
"Is it harder than modest weight loss?"
Not really—but you do need a good strategy. It requires the same basic tools (diet, exercise), but with a more targeted approach focused on blood sugar response, not just calories or pounds.
Have questions? We got answers. Email [email protected]

How did you like today’s newsletter? |

THAT’S A WRAP
[All original research data maintained but served with extra care ✨]
Here's to your health,
SP and Ava
from Prediabetes Mastermind





