- Prediabetes Mastermind
- Posts
- Can losing 20 pounds lower your HbA1c?
Can losing 20 pounds lower your HbA1c?
The science says yes (and here's your game plan)
Welcome back, health champions!👋
Ever wonder if losing weight actually moves the needle on your lab results?
Today we're diving into the connection between your scale and your A1C—and why losing just 10 pounds could be the game-changer you've been looking for. We're talking real numbers, real science, and a real plan that doesn't involve crash diets or gym obsessions.
In today's health guide:
Why your weight literally shows up in your blood work
The magic number that drops A1C by half a point
Your no-nonsense action plan
Go-to meal ideas for prediabetics
BEST FINDS
These blood sugar stability powerhouses are designed for easy batch cooking and sustained energy throughout your week. Turkey Taco Lettuce Wraps - High in protein, low in carbs, packed with fiber from veggies; Zucchini Stir-fry with Chicken - Lean protein and low-GI veggies with healthy fat if cooked in avocado or olive oil; Peanut Tofu Stir Fry With Broccoli, Peppers, and Quinoa - Plant-based protein, fiber, antioxidants; tofu helps with satiety; Chickpea and Spinach Curry - Chickpeas = fiber + protein; anti-inflammatory spices like turmeric, cumin; Black Bean Stuffed Sweet Potatoes - Natural sweetness balanced with fiber and protein; Hearty One-Pot Lentil Stew - Lentils offer slow-digesting carbs, fiber, and plant-based protein.
Can Losing 20 Pounds Actually Lower Your A1C?
Short answer: Absolutely. If you're a 180-pound woman, losing 20 pounds means an 11% weight loss—and that could drop your A1C by half a point or more, slashing your diabetes risk by nearly 60%.
Why Your Weight Shows Up on Your Lab Report
Here's what's happening behind the scenes: Your A1C measures your average blood sugar over the past three months. Think of it as your glucose report card.
But here's the kicker—extra weight, especially around your midsection, directly drives up that number. When you carry excess belly fat (the kind that wraps around your organs), it disrupts your metabolism through multiple pathways:
releasing inflammatory chemicals
altering hormone production
flooding your system with fatty acids
all of which work together to make your cells resistant to insulin.
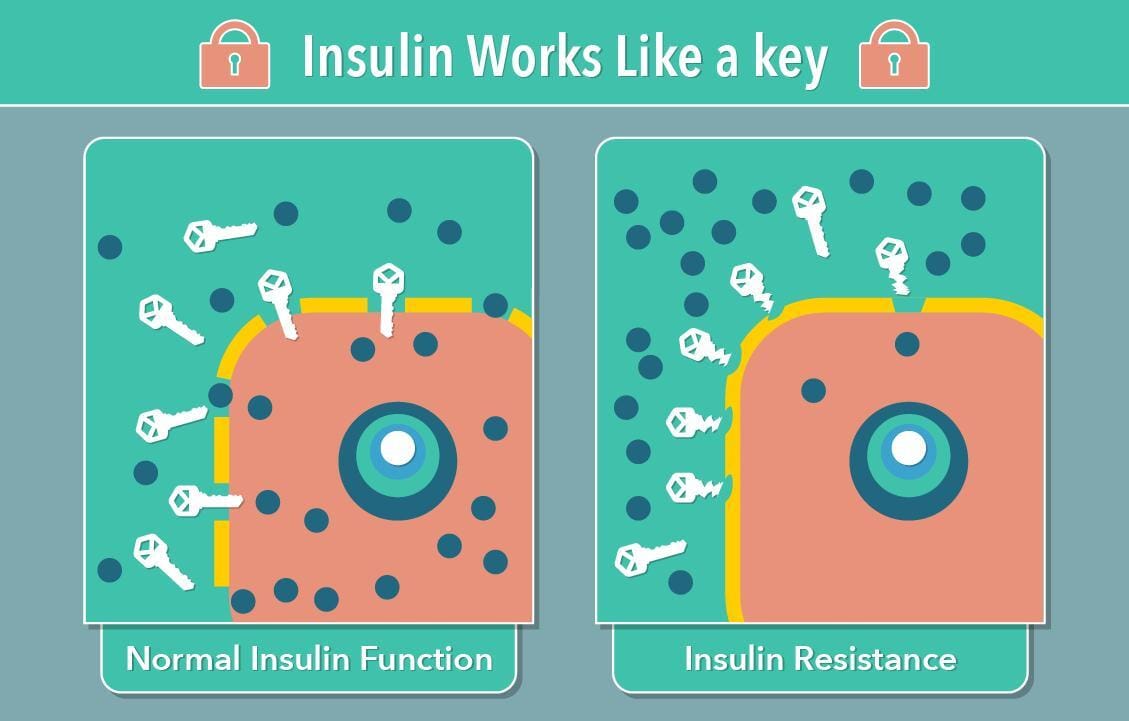
Picture insulin as a key trying to unlock your cells so glucose can enter. With insulin resistance, those locks get rusty. Your pancreas has to pump out more insulin just to keep blood sugar stable. Eventually, your blood sugar starts creeping up—and so does your A1C.
The Magic Numbers That Actually Move the Needle
The research shows clear benefits from modest weight loss. The CDC's landmark study found that losing just 5-7% of your body weight cuts your diabetes risk by 58%. That's only 10-14 pounds if you weigh 200 pounds.
For people who already have diabetes, losing 5% of your weight typically lowers A1C by about half a point. Since doctors can detect changes as small as 0.3%, every bit counts.
Here's what this looks like in real numbers:
If you weigh 150 pounds: losing 8-10 pounds = 5-7%
If you weigh 200 pounds: losing 10-14 pounds = 5-7%
If you weigh 250 pounds: losing 12-18 pounds = 5-7%
The bottom line: Studies show that people with diabetes see about a 0.05% drop in A1C for every pound lost. That means losing 10-20 pounds can make a real difference—not just wishful thinking, but proven results.
One encouraging finding: Women who lost more than 5% of their body weight were much more likely to get their A1C below 6.5%—the number that separates prediabetes from normal blood sugar.
How Weight Loss Actually Fixes Your Blood Sugar
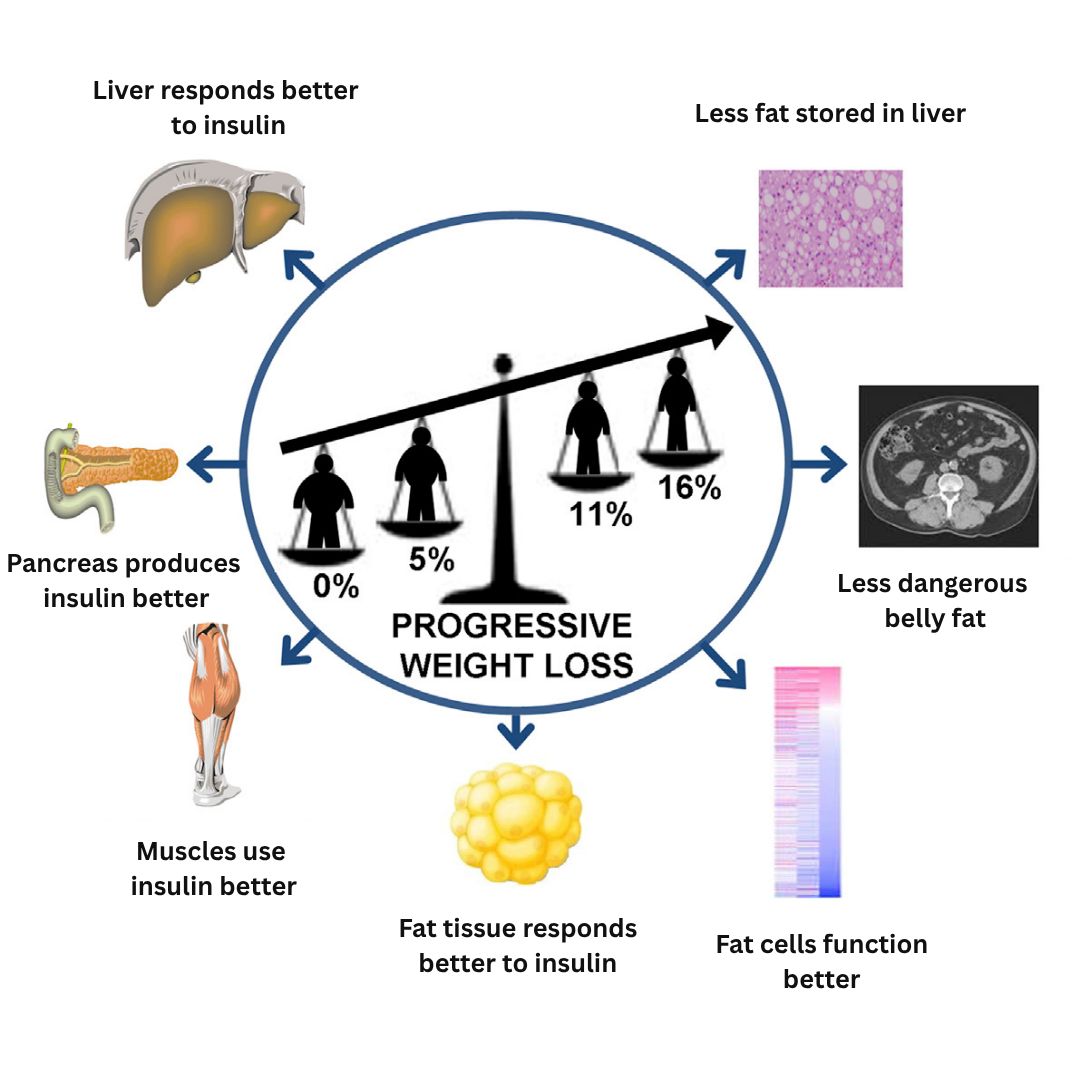
The magic happens through several pathways working together:
Less inflammation:
Losing belly fat reduces inflammatory chemicals in your bloodstream, allowing insulin to work more effectively throughout your body.
Liver efficiency:
Your liver produces glucose throughout the day. When you lose weight, your liver becomes more sensitive to insulin's signal to reduce glucose production—which is why fasting blood sugar often improves within weeks.
Muscle efficiency:
Even modest weight losses dramatically improve how your muscles take up glucose from your bloodstream. Translation: your body becomes more efficient at clearing sugar after meals.
Pancreatic relief:
With improved insulin sensitivity, your pancreas doesn't have to work as hard to produce insulin, helping preserve its function over time.
Why Fat Loss—Not Just Weight Loss—Matters Most
When losing weight, it's important to lose fat, not muscle. This matters for your A1C because muscle tissue is your body's largest glucose disposal site.
The research: A large study of over 13,000 adults found that increasing muscle mass by just 10% was linked to an 11% reduction in insulin resistance and a 12% decrease in prediabetes risk.
Muscle preservation strategies that work:
Protein timing matters:
Spread your protein intake throughout the day with 25-30 grams at each meal
Resistance training is non-negotiable:
Just two sessions per week of resistance exercise effectively prevents weight-loss-induced muscle loss. Cardio alone doesn't provide the same protection.
Leucine-rich foods:
Include Greek yogurt, eggs, cottage cheese, and lean meats—these contain high amounts of leucine, an amino acid that directly stimulates muscle protein synthesis.
Your Day-to-Day Prediabetes Reversal Game Plan
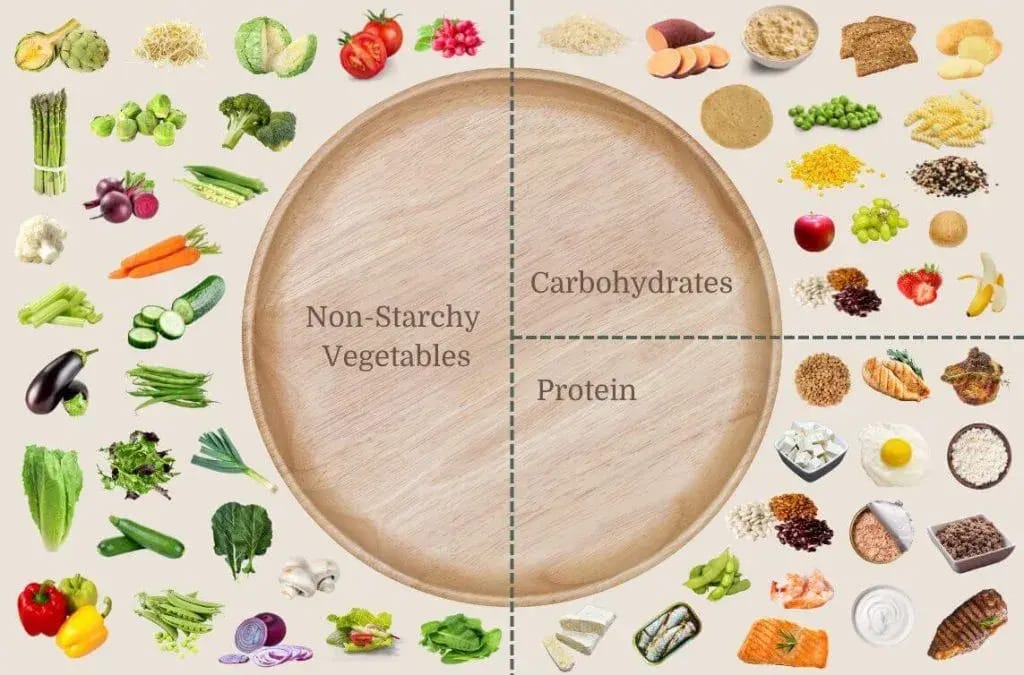
Smart Plate Strategy
Skip the complicated meal plans. Focus on this simple formula:
Half your plate: non-starchy vegetables
One quarter: lean protein
One quarter: high-fiber carbohydrates
Aim for 25-30 grams of protein at each meal to protect your lean muscle mass while losing weight.Read our article Carb Cravings + Blood Sugar Spikes? Here's Your Protein Solution
One simple swap that adds up: Replace sugary drinks with flavored seltzer or unsweetened tea. This single change can eliminate 200-300 calories daily without feeling deprived. Read our article Slash Your Hidden Sugar Intake by 300%
Which diet pattern works best for you is highly personal. Several community members have achieved lasting results with a Mediterranean-style approach, while others have used ketogenic diets and intermittent fasting for periods of accelerated progress. Read our complete guide Your Action Plan to Lower HbA1c to discover which approach aligns with your lifestyle and goals.
Movement That Actually Fits Your Life
The goal is at least 150 minutes of moderate activity per week plus two strength training sessions.
Juggling work and family? Try "exercise snacking": three 10-minute walks throughout the day work just as well as one 30-minute session. Read Walk Away from Prediabetes: 10-Minute Strategies for Busy Women
Sleep and Stress: The Hidden A1C Saboteurs
Aim for 7-9 hours of sleep nightly. Research shows that sleep deprivation significantly increases insulin resistance. When you're sleep-deprived, your body produces more cortisol and ghrelin (the hunger hormone), making weight loss infinitely harder.
Try this before meals: Five minutes of box breathing (inhale for 4, hold for 4, exhale for 4, hold for 4). This simple technique lowers cortisol and reduces stress-driven snacking. Read Prediabetes Is Affecting Your Mood (Here's How to Fix Both)
Track Progress Without Becoming Scale-Obsessed
Pay attention to non-scale victories that signal improving insulin sensitivity:
Steady energy at 3 PM instead of crashes
Fewer sugar cravings
Clothes fitting more comfortably around your waist
Navigate Common Roadblocks Like a Pro
When weight loss stalls (often within 2-4 weeks):
This is metabolic adaptation - your body's natural response to defend against weight loss. Combat it with multiple strategies: add resistance training sessions, increase protein intake, consider temporary diet breaks to reset metabolism, or make small stepwise calorie adjustments.
Social eating challenges:
Use the "half-plate veggie" rule at restaurants, volunteer to choose where your group eats, and order your drink first (make it water or unsweetened tea).
Maria, a 42-year-old teacher, lost 18 pounds in five months by stacking simple habits: brief walks after each meal, swapping her sugary drinks for sparkling water with lemon, fitting in quick strength exercises at home between tasks, and batch-cooking on Sundays. Her A1C dropped from 6.4% to 5.9%
Have a story? Share your small wins - we might feature you next! Email [email protected]
Normal-Weight Women with Prediabetes
If you're thinking "But I'm not overweight—how does this apply to me?" you're not alone. Research shows that people with normal BMI can still have prediabetes or diabetes, a condition sometimes called "metabolically obese, normal weight" or "skinny fat".
This means having a body mass index within the normal range, but a high proportion of fat to lean muscle—typically more than 25% body fat in males and 35% in females.
Your action plan if you're normal weight with prediabetes:
Focus on resistance training: Building muscle mass improves glucose disposal even without weight loss
Prioritize protein: Aim for the same 25-30g per meal to support muscle building
Target visceral fat: Even small reductions in waist circumference can improve insulin sensitivity
Consider body recomposition: Losing fat while gaining muscle can improve your metabolic health dramatically, even if the scale doesn't change
Consider partnering with a registered dietitian or joining a CDC-recognized Diabetes Prevention Program for accountability and personalized guidance.

How did you like today’s newsletter? |

THAT’S A WRAP
[All original research data maintained but served with extra purpose ✨]
Here's to your health,
Ava and Swapneeta
from Prediabetes Mastermind





